In the last Byte I examined implant location parameters that will lead to optimal outcomes for patients. As a recap I reviewed ideal implant location for esthetic and functional needs and discussed the importance and benefits of provisional implant restorations. In this edition I will focus on how to plan for implant restorations and then communicate your plan for the implant position to the surgeon, or yourself if you place implants.
The Planning Process
In recent times much attention has been given to “restoratively driven” implant placement. It is now the standard and begins from the planned final restoration, whether single tooth or complete denture. What are the most important aspects to take into consideration when planning for implants to replace single or multiple teeth?
- Patient-centered therapy
Most dental consumers are aware they have several options to replace missing teeth. Patients rely on us to help them make informed decisions to meet their goals. Ask your patient why they are seeking treatment and what they want to achieve by going through dental implant therapy. It is unfair and unethical to suggest only treatment modalities within our comfort zones or that patients have seen advertised when these may not be in their best interest.
2. Overall treatment plan
There should be no pressure to give a patient a solid answer for their planned procedures in a single visit. Proper planning, even for single teeth, is crucial and should include several diagnostic steps. These include intra- and extra-oral patient photographs, diagnostic impressions or intraoral scans, and appropriate radiographs including a CBCT. Items that need to be factored into a patient’s overall treatment solution include:
- Type of final restoration (cement or screw-retained)
- Surgical guide (CAD/CAM generated or laboratory fabricated)
- Future Whitening or esthetic procedures for anterior restorations
- Provisional implant restoration(s)
- Oral orthotic or nightguard appliance
Patients should understand the process required for you to fabricate a successful implant restoration. This may also include adjunctive soft and hard tissue grafting if it will improve the final outcome.
3. Restorative requirements
a. Inter-tooth spacing
This is entirely dependent on the location of the tooth to be replaced. Studies show a minimum of 1.5mm of space between an adjacent tooth and implant results in a more manageable scenario. For a posterior tooth this space should be greater to facilitate a normal shaped crown. If an implant is placed too close to a tooth there is a higher chance of biological complications and it becomes more difficult to restore the implant.
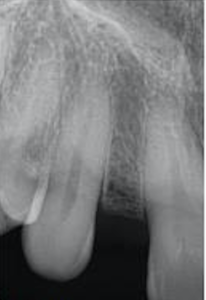
Fig 1. Insufficient Intertooth Spacing for Implant Therapy
b. Interarch spacing
Implants have additional components that teeth do not. Additional space for an abutment and abutment screw must be taken into consideration. 5mm is the minimum space necessary to be able to accommodate all of the implant components AND the restorative materials for a normal implant crown. Looking at this space BEFORE the implant is placed is absolutely necessary. If there is a lack of space consider adjusting the opposing tooth, having the implant placed deeper, or discussing different treatment modalities, like orthodontics, with your patient if the vertical dimension is compromised.
c. Implant depth
In the previous Byte general parameters were listed for anterior implants. To review implant depth should be1:
– 2.5 – 3mm apical to the desired gingival zenith in the anterior and premolar regions. Molar implants may not have the same esthetic requirements but may require a similar depth in order to recreate hygienic interproximal contours.
– 2mm lingual to the desired gingival zenith for anterior implants. Posterior implants should be centered as much as possible within the alveolar ridge. Several studies show the importance of this position for long-term stability of facial bone. In addition, with screw-retained crowns coming into favor, this position is important so the restoring dentist has more control over the final restoration.

Fig 2. Clear surgical stent with desired gingival zenith outlined in blue
Once you have planned your implant restoration(s) you can move forward with communicating your desired implant position. We have verbal and non-verbal modes to do this. Personally I find both to be necessary to ensure that everyone is on the same page. Contact the surgeon and schedule a time to review the case, or if you are placing ensure you have anticipated any surprises. The non-verbal communication should be in the form of a surgical guide. Even for implants that everyone may perceive as “slam dunks” positioning can still go awry during surgery. The prosthodontic literature is replete with publications describing various techniques for making surgical guides. The technique is not as important as a guide being fabricated AND tried in prior to surgery. If you do both, your surgeon will know you have planned your implant restoration. The surgeon will need to communicate any deviations from the guide if they occurred during surgery so you can plan appropriately for your final restoration.
In conclusion, careful planning and fabrication of a well-fitting surgical guide will aid in proper implant positioning and will communicate to all parties your intended final restoration. With the increasing use of implants to replace missing teeth we want patient outcomes to be positive and not centered around complications that can be avoided. As always I am available to consult with you on specific cases you have questions about and welcome referrals for patients you do not feel comfortable treating.
Dr. Emily Batson is a native of Colorado Springs, CO. She is a graduate of Indiana University School of Dentistry, and served in the United States Army following dental school. She completed her specialty training in Prosthodontics at the University of North Carolina at Chapel Hill.
References:
- Cooper LF, Pin-Harry O. “Rules of Six” – Diagnostic and Therapeutic Guidelines for Single-Tooth Implant Success. Comp Cont Dent Education. Feb 2013.
