Combination Syndrome Revisited
Recently I reviewed diagnostic casts for a patient receiving a maxillary complete denture and noted some characteristic features of Combination Syndrome. Ironically, I looked at casts from another patient opposing a mandibular implant overdenture and saw a few striking similarities. In this edition of the Byte I will review one of dentistry’s more popular “Syndromes” and highlight where and why we continue to see this. I will also discuss aspects to consider when treating someone with Combination Syndrome.
A Review of Combination Syndrome
Dr. Ellsworth Kelly was the first to name and publish on Combination Syndrome in 1972 in the Journal of Prosthetic Dentistry. His article discussed 5 key features of patients who have Combination Syndrome, also termed Anterior Hyperfunction Syndrome, or Kelly Syndrome.
- Loss of bone from the maxillary anterior region
- Overgrowth of the maxillary tuberosities
- Papillary hyperplasia of the palatal mucosa
- Extrusion of the mandibular anterior teeth
- Loss of bone on mandibular posterior regions (noted under RPD bases)
It is difficult to quote exact percentages of individuals who suffer from Combination Syndrome, as there are individual factors at play that cannot always be controlled. For example, how long has the patient been edentulous and how traumatic were extractions or tooth removal on the remaining bone. In addition, with implant therapy, we may continue to see some of the attributes of combination syndrome but not always all five features.
Treatment planning for patients with Combination Syndrome
Patients don’t typically walk into our offices saying, “I am here for help with my Combination Syndrome”. Most of these folks come in when a denture no longer fits to their satisfaction, or they have noticed enough changes in function and appearance they feel they are ready for a new prosthesis. Patients with implant retained mandibular prostheses may complain of a loose maxillary denture due to continued resorption of the Type II/III bone seen in the anterior maxilla. First things first, examine the edentulous arch carefully, using a mirror to look at the tissues and remaining architecture and the end of the mirror to lightly probe tissues for hypertrophy and/or mobility. Note the color of the tissues and if any erythema is present. Have the patient smile both with and without the maxillary denture. Make a note if you can see the maxillary ridge at all, or if only posterior regions show (possible tuberosity overgrowth). This often relates to a reversed occlusal plane seen when the patient smiles with their denture. We may only see the mandibular anterior teeth because of supraeruption and never see the maxillary anterior teeth because of a combination of wear, lip position, and where the denture has continued to seat itself due to bone resorption. These are the attributes to point out to a patient during treatment planning so you can better accommodate any requests of the patient regarding a new denture. Have the patient decide how important tooth display will be. This may mean treatment of the lower arch, even though they just came for treatment of the maxillary arch. For individuals wanting implant therapy, mounted diagnostic casts will be imperative to ensure there is enough restorative space in the posterior maxillary regions for the implants and prosthesis. Lastly, patients should be reminded of maintenance with dentures. Relines and remakes need to be expected. For the edentulous individual they should be informed of proper home care and annual exams to inspect dentures and tissues. In summary, treatment considerations should include:
- Changing of esthetics – multiple wax try-ins may be needed to ensure the position of the maxillary anterior teeth can be set in a satisfactory position. Recall that the anthropometric average value of the maxillary anterior teeth from the anterior maxillary vestibule is 22mm.
- Change in function – if there is excessive hypertrophic or inflamed tissue, or excessive overgrowth of the tuberosity region, the patient may need a surgical intervention with tissue reduction, or a temporary tissue conditioner with their existing prosthesis.
- Treatment for the opposing arch – if the mandibular anterior teeth are too far extruded or in poor condition, consider removal of the remaining teeth and a two-implant mandibular overdenture. An alveoloplasty of the mandibular anterior ridge of often necessary to allow for sufficient restorative space and to prevent the same esthetic appearance from happening again.
Case Study: A 58 yo female was referred for treatment of the maxillary arch. Her dental history included removal of the maxillary teeth at age 30 and she was wearing her first and only denture. The mandibular teeth displayed supraeruption but were in good condition. The patient desired more tooth display and whiter teeth. A new maxillary denture was fabricated after tissue conditioning was performed with her existing prosthesis.

Fig. 1 Lack of anterior tooth display with existing denture

Fig 2. Mandibular teeth show supraeruption; note thin anterior maxillary ridge
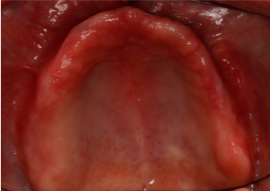
Fig 3. Erythematous tissues noted

Fig 4. New maxillary denture correcting midline and tooth display
I hope this edition of the Byte has been helpful. As always, I appreciate your referrals and am available to discuss any clinical scenarios you may have questions about. I can be reached by phone at 719-576-4247.
Dr. Emily Batson is a native of Colorado Springs, CO. She is a graduate of Indiana University School of Dentistry and completed her prosthodontic residency at The University of North Carolina at Chapel Hill. She maintains a full-time private practice limited to prosthodontics in Colorado Springs.
References:
- Kelly E. Changes caused by a mandibular removable partial denture opposing a maxillary denture. J Pros Dent 1972; 27.