The Batson Byte
“a unit of dental insight for the curious practitioner”
Emily R. Batson DDS, MS
The many ways of building bridges
I went for a run in the snow recently and decided to wear an old familiar pair of running shoes. As I was slipping around trying to maintain my balance, I was reminded that I needed to take myself off auto-pilot. I had become used to running on predictable surfaces with newer shoes, but quickly realized I needed to change my focus in order to adapt and not fall. Building bridges that connect dental implants requires a similar mindset, as there can be no “auto-pilot” setting in restoring these. In this issue of the Byte I will discuss several ways that multiple dental implants can be restored and review methods to help accomplish these clinical presentations.
The Original Implant Bridge
Professor Brånemark can be credited with developing the ideas behind the first dental implant bridge. Our first dental implant restorations were placed in edentulous mandibles, with a minimum of three fixtures connected by a cast metal bar layered with acrylic.1 It was not until the 1980’s that we started using dental implants to replace single teeth, and then eventually multiple teeth in separate quadrants. During the first twenty years of implant placement, our parts and pieces were somewhat rudimentary. We did not have access to the array of stock or CAD/CAM abutments we do today, so each connecting component was “custom”. We were also dealing primarily with external hex implants. This type of implant design can be handy when connecting multiple implants that are somewhat divergent, as it has a very short retentive element (the hex) but it also has very little anti-rotation effect, thus the screw is doing most of the retentive work. Fast forward a few more years to implants that had an internal connection (internal hex, morse taper, lobes, etc.) These have allowed for many other discussions to take place, including better bone and soft tissue outcomes, and potentially better restorative outcomes. As we are seeing most of the external hex implants go out of fashion, what are our options for connecting multiple implants?
Implant Level vs. Abutment Level Bridges
The words implant level or abutment level are applied to both single unit implant restorations and those connecting multiple implants. Let’s look at the in’s and out’s of both.
- Implant Level – this term connotates a restoration connecting directly to the implant interface, meaning the abutment and restoration are typically made as one piece. The most common way of seeing this is a cast-to screw-retained implant restoration. Implant bridges can be fabricated this way however, implant angulation and connection are the two main variables that will determine whether this is the most feasible type of restoration. For external hex implants that are relatively parallel, implant level bridges can be a great design. I’ll discuss engaging vs. non-engaging components later, but non-engaging components frequently need to be utilized for implant level restorations in order to achieve a passive fit, especially with internal connection implants.
- Abutment Level – this term is used to describe a restoration that will be connected to abutments. Abutments can be stock, custom, engaging or non-engaging, or a combination of any of these. The restoration will connect to an abutment or abutments. It is important to remember that two sets of screws may be involved here, unless there is a cement interface. The simplest abutment level FPD would involve two stock or custom abutments and a cemented FPD over these.
Below is an example of an Implant Level FPD
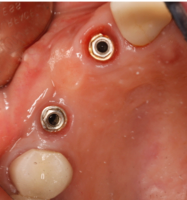
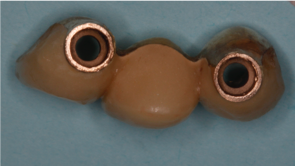
Fig 1. Note external hex implants and non-engaging abutments within the PFD
Below are examples of Abutment Level FPDs


Fig 2. Note screw-retained PFM FPD using multi-unit abutments


Fig 3. Three-unit FPD cemented over custom abutments
With so many different materials and technologies available there are several options available to make implant bridges. Abutments can be titanium, zirconia, or a combination alloy. FPDs can be metal based or ceramic based. Is there one material better than another? Unfortunately, the literature does not demonstrate one material being superior to another. We likely will not know the outcomes of our decision until years down the road.
I’ll continue the discussion of implant bridges in the next edition, where I will discuss non-engaging vs. engaging components, screw-retained vs. cement retained options, and materials. I’ll also talk briefly about fabrication methods and impression techniques. I hope this Byte has been helpful.
As always, I appreciate your referrals and am available to discuss any clinical scenarios you may have questions about. I can be reached by phone at 719-576-4247.
Dr. Emily Batson is a native of Colorado Springs, CO. She is a graduate of Indiana University School of Dentistry, and served in the United States Army Dental Corps. She completed her specialty training in Prosthodontics at the University of North Carolina at Chapel Hill. She maintains a full-time private practice limited to prosthodontics in Colorado Springs.
References:
- Branemark, PI. ”Tissue-Integrated Prostheses; Osseointegration in Clinical Dentistry. Quintessence, 1985.
